BUSTED! Even bogus anti-abortion 'study' shows medication abortion is safer than pregnancy, birth
By the numbers, anti-choicers' own pseudoscience supports increasing abortion access—not restricting it.
In 2025, the Ethics in Public Policy Center (“EPPC”), a conservative think tank with a record of hostility to medication abortion, released an analysis of insurance data purporting to show that serious adverse events occur more frequently than reported by the United States Food and Drug Administration (“FDA”) and, based on the results, that the FDA should reinstate prior restrictions on mifepristone prescriptions.
Since its release, the analysis has come under heavy criticism for fundamental problems with its design and methodology that seriously undermine EPPC’s claim that medication abortion has more risk in real world settings than previously disclosed.1 The analysis does not reliably identify patients who have taken medication abortion and misclassifies serious adverse events. At best, the analysis demonstrates that if you count more outcomes as serious adverse events, you will get a higher rate of serious adverse outcomes. Furthermore, EPPC does not identify the data that it uses and is not sufficiently specific about how it identifies serious adverse events for their results to be validated. EPPC’s analysis is not a methodologically rigorous, evidence-based analysis. It’s more like an anti-abortion press release with a chart to make it seem credible.
The safety and efficacy of medication abortion is supported by evidence from hundreds of clinical trials and decades of safety data based on real world use.2 That has not been called into question by a shady analysis from an anti-abortion think tank that won’t even show its work.
For pregnant patients, medication abortion is far safer than staying pregnant and giving birth.
Even if the complication rates reported by EPPC were valid, medication abortion is still far safer than the alternative: staying pregnant and giving birth. EPPC presents the risks of medication abortion in isolation, without stating the obvious: without access to medication abortion, many people who would otherwise end their pregnancies will continue pregnancy. The anti-abortion movement is counting on it.
Like any other treatment regimen, any assessment of the risks of medication abortion must account for the alternatives to treatment.3 For pregnant patients, continuing pregnancy is not a neutral background: the same physiological processes that sustain fetal life and development also expose pregnant patients to pain, injury and escalating medical risk. Because these risks arise from continuation of pregnancy, many of these risks can be mitigated or avoided by ending pregnancy promptly when a pregnant patient has decided that they do not want to continue pregnancy. Moral objections to abortion do not alter medical risks. The safety of medication abortion must be evaluated against the risk of continuing pregnancy.
Even assuming EPPC’s results did not wildly overstate the risks of medication abortion (they do), EPPC’s results would still demonstrate that medication abortion is far safer for pregnant patients than continuing pregnancy and giving birth.
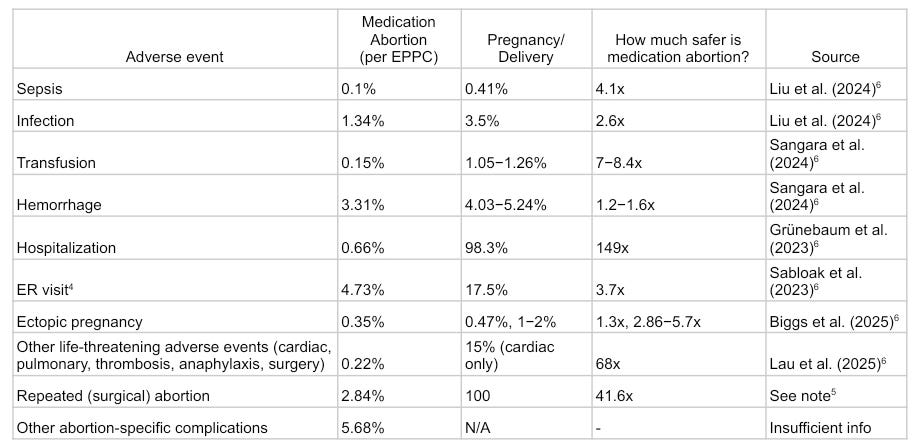
The below graph compares the EPPC's numbers with the risks associated with continuing pregnancy and giving birth (see footnotes456).
Click here for the document version of the graph.
The risks associated with continuing pregnancy and birth that are presented in the graph above are reported conservatively, by design. Results have been pulled from studies that focus on risks related to deliveries and live birth to ensure that no abortion-related risks were attributed to risks related to pregnancy and birth. As a result, the risks listed above generally exclude risks related to miscarriage, stillbirth, and complications earlier in pregnancy and cannot account for the full spectrum of risks associated with continuing pregnancy.
Even by EPPC's inflated figures of mifepristone “complications,” medication abortion is still far safer than continuing pregnancy and giving birth.7 —The only way for anti-choicers to argue that medication abortion is “unsafe” is to pretend that continuing pregnancy and giving birth has no risk. But pretending pregnancy and birth are risk free is not a valid way to assess the safety of medication abortion for pregnant patients.
While pregnancy is not a disease, it is a condition that exposes patients to serious health risks. As the above graph demonstrates, limiting access to medication abortion necessarily puts pregnant patients at greater risk.
None of the ‘safety’ restrictions on medication abortion that EPPC proposes provide any safety benefit. In fact, restrictions on medication abortion in general have always reflected a pattern of over-regulation stemming from the controversial nature of abortion (“abortion exceptionalism”), rather than reflecting the inherent safety of the drug.8
Requiring an in-clinic visit does not reduce any pharmacological risk related to mifepristone, and the delay that would result from such a requirement would only increase risk to pregnant patients. While both medication abortion and procedural abortion are safe for pregnant patients at all stages of gestation, with low risks of complications, risks increase as gestation progresses.9 Delays can mean the difference between accessing medication abortion or needing a procedural abortion, which can significantly increase the cost of care, especially for patients in regions where access to abortion is restricted, and push patients even further in gestation. A requirement for in-person visit access to abortion offers no benefit to pregnant patients and by creating barriers to abortion access only increases medical risk to pregnant patients.
EPPC’s analysis does not provide a valid basis for its conclusions or its policy recommendations. But since its release, the anti-abortion movement has tried to use EPPC’s analysis to call for restrictions on abortion. The anti-abortion movement is calling for policies that would put patients at greater risk and saying that it’s for their safety. Moral objections to abortion do not excuse dishonesty about medical risk.
Restrictions on medication abortion access put pregnant patients at greater risk. Every lie, every evasion, every distortion, every context-free assertion made by the anti-abortion movement or its political collaborators about the safety of medication abortion should be seen for what it is: a direct reflection of how little the safety of pregnant patients matters to them.
Comment Letter of 263 Reproductive Health Researchers on Mifepristone Shared System Risk Evaluation and Mitigation Strategy, Docket No. FDA-2025-P-1242-0004 (Oct. 31, 2025), https://www.regulations.gov/comment/FDA-2025-P-1242-0004; Letter from Soc’y for Fam. Plan. to Martin Makary, Comm’r, FDA, (May 2, 2025), https://societyfp.org/wp-content/uploads/2025/05/SFP-Letter-to-Commissioner-Makary_5.2.2025.pdf; Glenn Kessler, Fact Checking a Study on the Safety of the Abortion Pill - The Washington Post, Washington Post (May 12, 2025), https://www.washingtonpost.com/politics/2025/05/12/abortion-pill-medication-abortion-study-mifepristone/; Kimberly Heatherington, Experts Flag Concerns over EPPC Study on Dangers of Pill Used in Miscarriage Care, Abortion, Catholic Review (May 21, 2025), https://catholicreview.org/experts-flag-concerns-over-eppc-study-on-dangers-of-pill-used-in-miscarriage-care-abortion/; Marisha Goldhammer, “Flawed” Paper Overstates Health Risks of Abortion Pills: Experts, (May 12, 2025), https://factcheck.afp.com/doc.afp.com.444Z863.
Sophie Dilek et al., The US Food and Drug Administration’s Regulation of Mifepristone, JAMA (2026), https://jamanetwork.com/journals/jama/fullarticle/2843710.
U.S. Food & Drug Admin., Benefit-Risk Assessment for New Drug and Biological Products; Guidance for Industry; Availability, Federal Register (Oct. 20, 2023), https://www.federalregister.gov/documents/2023/10/20/2023-23161/benefit-risk-assessment-for-new-drug-and-biological-products-guidance-for-industry-availability.
GRAPH NOTE 4:
Visits to the emergency room should not be counted as serious adverse events in and of themselves for either pregnancy or abortion without more information. U.S. Food & Drug Admin., What Is a Serious Adverse Event?, U.S. Food & Drug Admin. (May 18, 2023), https://www.fda.gov/safety/reporting-serious-problems-fda/what-serious-adverse-event. A majority of abortion-related visits the ER require observation care only. Ushma D. Upadhyay et al., Abortion-Related Emergency Department Visits in the United States: An Analysis of a National Emergency Department Sample, 16 BMC Medicine (2018).
GRAPH NOTE 5:
EPPC counts procedural abortion as an adverse event. A patient who gets an abortion that is not medication abortion must get a procedural abortion instead, so their “risk” of procedural abortion is 100%.
GRAPH REFERENCES:
Biggs, M. A., Armstrong, M. A., Tucker, L.-Y., Kaller, S., Rabbani, J., Lee, J. W., Chillemi, G., & Grossman, D. (2025). Incidence of Ectopic Pregnancy and Diagnostic Accuracy of Ectopic Pregnancy Screening Criteria Among People Seeking Versus Not Seeking Abortion: A Retrospective Case-Control Study. Women S Health Issues, 35(6). https://doi.org/10.1016/j.whi.2025.08.006
Grünebaum, A., Bornstein, E., McLeod-Sordjan, R., Lewis, T., Wasden, S., Combs, A., Katz, A., Klein, R., Warman, A., Black, A., & Chervenak, F. A. (2023). The impact of birth settings on pregnancy outcomes in the United States. American Journal of Obstetrics and Gynecology, 228(5, Supplement), S965–S976. https://doi.org/10.1016/j.ajog.2022.08.011
Hall, J. B., & Anderson, R. T. (2025, May 10). The Abortion Pill Harms Women: Insurance Data Reveals One in Ten Patients Experiences a Serious Adverse Event - Ethics & Public Policy Center. Ethics & Public Policy Center. https://eppc.org/publication/insurance-data-reveals-one-in-ten-patients-experiences-a-serious-adverse-event/
Lau, E. S., D’Souza, V., Zhao, Y., Reeder, C., Goldberg, R., Flores, M., Economy, K. E., Maddah, M., Khurshid, S., Ellinor, P. T., & Ho, J. E. (2025). Contemporary Burden of Cardiovascular Disease in Pregnancy: Insights From a Real-World Pregnancy Electronic Health Record Cohort. Circulation, 152(15). https://doi.org/10.1161/circulationaha.125.074692
Liu, L. Y., Friedman, A. M., Goffman, D., Nathan, L., Sheen, J.-J., Reddy, U. M., D’Alton, M. E., & Wen, T. (2024). Infection and Sepsis Trends during United States’ Delivery Hospitalizations from 2000 to 2020. American Journal of Perinatology, 41(13), 1767–1778. https://doi.org/10.1055/s-0044-1780538
Sabloak, T., Yee, L. M., & Feinglass, J. (2023). Antepartum Emergency Department Use and Associations with Maternal and Neonatal Outcomes in a Large Hospital System. Women’s Health Reports, 4(1), 562–570. https://doi.org/10.1089/whr.2023.0072
Sangara, R. N., Matsushima, K., Matsuzaki, S., Yao, J. A., Yu, E., Mandelbaum, R. S., Grubbs, B. H., Incerpi, M. H., Ouzounian, J. G., & Matsuo, K. (2024). Temporal trends of obstetric hemorrhage and product-specific blood transfusion at time of delivery. American Journal of Obstetrics and Gynecology, 231(4), e139–e145. https://doi.org/10.1016/j.ajog.2024.06.012
It is not mentioned in the EPPC analysis but the mortality risk of mifepristone-associated death is 0.48/100,000 abortions. Post marketing event reports include deaths that are not causally related to mifepristone; excluding deaths that are not plausibly related to medication abortion (like deaths from alcohol toxicity), the mortality risk of medication abortion is 0.29 deaths/100,000 abortions. The live birth mortality rate is approximately 8.8 deaths/100,000 live births. The risk of death from medication abortion is somewhere between 18 and 30 times lower than the risk of death related to child birth. Mifepristone U.S. Post-Marketing Adverse Events Summary through 12/31/2024 (2025); Elizabeth G. Raymond & David A. Grimes, The Comparative Safety of Legal Induced Abortion and Childbirth in the United States, 119 Obstetrics & Gynecology 215 (2012).
Mifeprex REMS Study Group, Sixteen Years of Overregulation: Time to Unburden Mifeprex, 376 N Engl J Med 790 (2017); Greer Donley, Medication Abortion Exceptionalism, 107 Cornell Law Review 627 (2022).
Isabel Fulcher et al., Changes to Parental Consent Requirements for Abortion in Massachusetts and Impact on Timeliness of Care for Adolescents Aged 16 to 17 Years, 115 Am J Public Health 397 (2025).