How We Know Abortion Is Safer Than Birth
Demonstrating abortion is safer than birth, even if real world data isn't perfect
To provide clarity, this report will provide a brief overview of how deaths related to pregnancy, birth and abortion are tracked by the CDC, review how Raymond & Grimes generated the numbers that led to the finding that abortion is 14 times safer than birth and why we can be confident that legal induced abortion is safer than pregnancy.
👤 GUEST POST
K. Brooks is a university researcher in the northeastern United States.
Outline
Calculating Relative Risk of Abortion and Live Birth
A. How Raymond and Grimes Calculated Risk of Death Related to Live Birth
B. How Raymond and Grimes Calculated the Mortality Rate Related to Legal Abortion
C. How Raymond and Grimes Calculated the Relative Risk of Live Birth to Legal Induced Abortion
⓵ Introduction and Purpose
The recent expansion of abortion bans has brought renewed attention to the relative safety of abortion compared to childbirth; since 1972, data and analysis indicates that the mortality rate from live birth is higher than the mortality rate from legal abortion (Cates et al., 1982; Coble et al., 1992; Grimes, 2006), with one well-cited analysis from authors Raymond & Grimes (2012) reporting that live birth has fourteen times the mortality rate of legal abortion. This study by Raymond and Grimes has been frequently cited by media and supporters of legal abortion as evidence that abortion bans expose pregnant people who would otherwise terminate their pregnancies to increased risk.
In the years since its publication, a number of opponents of legal abortion have challenged the results of the Raymond & Grimes analysis, arguing that methods and data sources used to calculate the relative risk of abortion either understate the risk of abortion or overstate the risk of birth (Calhoun, 2013; Ferrer, 2020; Reardon, 2012; Reardon et al., 2004; Skop, 2023, 2024).
However, these critiques share common errors: critics (1) misrepresent the data and (2) misinterpret the analysis conducted by Raymond & Grimes, and based on this misunderstanding, (3) claim that the conclusion that abortion is safer than birth is unwarranted or even biased.
To provide clarity, this report will provide a brief overview of how deaths related to pregnancy, birth and abortion are tracked by the CDC, review how Raymond & Grimes generated the numbers that led to the finding that abortion is 14 times safer than birth and why we can be confident that legal induced abortion is safer than pregnancy.
⓶ How the CDC Tracks Mortality Related to Pregnancy and Birth
The Centers for Disease Control and Prevention uses three primary systems to track deaths related to pregnancy and birth: National Vital Statistics System (“NVSS”), Pregnancy Mortality Surveillance System (“PMSS”), Maternal Mortality Review Information Application (“MMRIA”).1
🅐 Two Systems Are Used to Generate National Statistics to Track Mortality Related to Pregnancy and Childbirth: NVSS and PMSS
NVSS and PMSS are used to generate national statistics on deaths arising from or caused by pregnancy and birth.
■ CDC’s National Center for Health Statistics (“NCHS”) reports maternal mortality through NVSS.
■ CDC’s National Center for Chronic Disease Prevention and Health Promotion’s Pregnancy Mortality Surveillance System (“PMSS”) conducts epidemiological surveillance of pregnancy-related deaths.
National Vital Statistics System (NVSS)
The National Vital Statistics System (“NVSS”) is federally mandated to collect and publish national mortality data based on the cause of death identified on death certificates.
A maternal death is defined by the World Health Organization as, “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes” (National Center for Health Statistics, 2024). Traditionally, deaths related to induced abortion are counted as a type of maternal mortality; internationally, unsafe abortion is one of the leading causes of maternal death (WHO et al., 2023).
Maternal deaths, identified from the cause of death (ICD codes) listed on the death certificates filed in states’ vital statistics agencies, are compiled by the CDC using the National Vital Statistics System (NVSS) and reported as the official maternal mortality rate reported per 100,000 live births. This is the maternal mortality rate traditionally used to make historical and international comparisons (Gerberding, 2004).
Raymond and Grimes Did Not Use the NVSS to Compare Deaths Associated With Live Births and Deaths Associated With Legal Abortion
The official maternal mortality rate is useful for historical purposes and for making international comparisons, but the official maternal mortality rate is not comparable to the abortion-related mortality rate reported by the CDC.
NVSS counts all deaths attributed to obstetric or pregnancy-related causes within 42 days of the end of pregnancy (as identified on the death certificate). Maternal deaths for all pregnancy outcomes are counted in the official maternal mortality rate; for example, it includes deaths attributed to live birth, stillbirth, ectopic pregnancy, abortion (spontaneous and induced), molar pregnancies. Because maternal mortalities are identified using only the cause of death recorded on death certificates and because only deaths within 6 weeks of the end of pregnancy are counted, NVSS may significantly undercount maternal deaths (Cates et al., 1982; Coble et al., 1992; MacKay et al., 2005).
In calculating the rate of relative risk of live birth and abortion, Raymond and Grimes did not use data from NVSS; the authors based their analysis on deaths identified as “pregnancy-related” by PMSS.
Pregnancy Mortality Surveillance System (PMSS)
Since 1987, the CDC has tracked pregnancy-related deaths, deaths that occur during or within 1 year of pregnancy and that are caused by pregnancy complications using the Pregnancy Mortality Surveillance System (“PMSS”) (Centers for Disease Control & Prevention, 2024). PMSS uses epidemiological surveillance to identify pregnancy-related deaths by examining all deaths within a year of pregnancy.
To collect this information, CDC requests de-identified copies of death certificates for all deaths occurring during or within 1 year of pregnancy (pregnancy-associated deaths), regardless of the cause of death or duration of pregnancy from 52 reporting areas (the 50 states, New York City, and Washington, DC) (Berg et al., 2010). For deaths occurring within a year of a live birth or stillbirth, a copy of the matching birth or fetal death certificate is also requested.
Based on this data, pregnancy-related deaths, defined as a “death during or within 1 year of pregnancy that was caused by a complication of pregnancy, a chain of events initiated by pregnancy, or aggravation of an unrelated condition or event by the physiologic effects of pregnancy” are identified from the death records based of the review of clinically-experienced epidemiologists (Berg et al., 2010). CDC’s epidemiologists analyze death records (and on request, additional medical records, including autopsy records) and code information on the outcome of pregnancy, cause of death, and associated conditions and assess whether there is a causal relationship between pregnancy and death based on the clinical cause of death, the time interval between pregnancy and death, and the pathophysiology of complications in pregnancy (Berg et al., 2010).
▪︎ Not All Deaths Within a Year of Pregnancy Are Related to Pregnancy or Birth.
Death from a condition that is not unique to pregnancy is not considered “pregnancy-related” based solely on its occurrence within one year of pregnancy. A significant number of pregnancy-associated deaths reported to the CDC (deaths that are potentially pregnancy-related because they occur within a year postpartum) are not identified as causally related to pregnancy.2
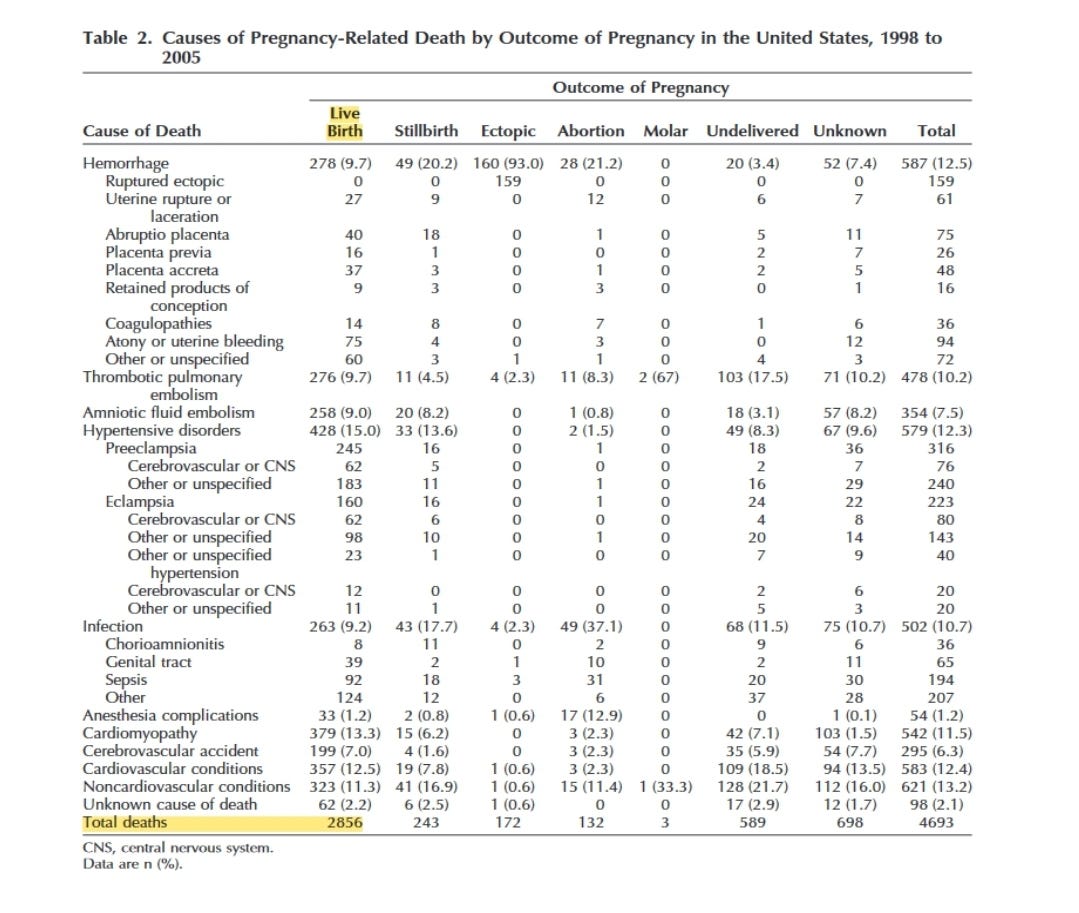
For example, in the 8-year period from 1998 to 2005, data for 9,988 potential pregnancy-related deaths were received by the Division of Reproductive Health. Of these, 4,693 deaths were found to be pregnancy-related (occurring during or within 1 year of pregnancy from a condition caused by or aggravated by the physiologic effects pregnancy); 5,151 were pregnancy-associated but not pregnancy-related (occurring during or within 1 year of pregnancy but from a condition caused by or aggravated by the physiologic effects pregnancy ) (Berg et al., 2010).3
▪︎ All Pregnancy-Related Deaths in PMSS Are Categorized by Pregnancy Outcome.
Each death identified as pregnancy-related is coded for the outcome of the pregnancy: live birth, stillbirth, ectopic pregnancy, abortion (spontaneous and induced), molar pregnancy, undelivered and unknown (Berg et al., 2010).4 The number of deaths related to legal induced abortion and live birth are both identified by PMSS, allowing more comparability between outcomes.
▪︎ Abortion-Related Mortalities Are Identified by the PMSS System.
Abortion-related mortalities, deaths related to spontaneous and induced abortions, are one of the pregnancy outcomes identified by the PMSS system.5 Abortion-related deaths are further classified as related to induced or spontaneous abortions, and induced abortions further classified as legal or illegal. From 1998 to 2005, an induced abortion was defined as a procedure “that is intended to terminate a suspected or known intrauterine pregnancy and produce a nonviable fetus at any gestational age”(Pazol et al., 2011); any abortion “performed by a licensed physician, or an appropriately licensed advanced practice clinician acting under the supervision of a licensed physician” was considered “legal” and an abortion performed by any other person was considered “illegal”(Pazol et al., 2011). Abortion-related death is defined as “a death resulting from a direct complication of an abortion (legal or illegal), an indirect complication caused by a chain of events initiated by an abortion, or aggravation of a preexisting condition by the physiologic or psychologic effects of abortion” (Pazol et al., 2011).
Based on the long standing recognition that abortion-related mortalities may not always be identified as abortion-related or pregnancy-related deaths on death certificates, identification of additional deaths that may be related to abortion are also obtained through “state vital records, public health agencies, maternal mortality review committees, health-care providers, private citizens and citizen groups, and media reports, including computerized searches of full-text newspaper and other print media databases” (Pazol et al., 2011).
▪︎ Cdc’s Active Surveillance of Abortion-Related Deaths Has Been Highly Effective in Identifying and Reducing Abortion-Related Mortality .
“CDC’s early and continued vigilance in conducting abortion surveillance, investigating abortion-related deaths, and studying the safety of abortion techniques has helped to virtually eliminate maternal mortality from abortion in the United States” (Rochat et al., 2011).
While critics have long claimed that CDC data on abortion-related mortality data is not sufficient, because states only report abortion-related deaths to NHCS voluntarily, the active epidemiological surveillance methods used by the CDC are considered far more accurate than methods of reporting that use only cause of death identified from vital records alone. A review by the American Medical Association found that using the mandatory reported data provided by states would only have identified 52% of abortion-related deaths, while CDC’s abortion surveillance system identified 94% of all abortion-related deaths (Coble et al., 1992). Intense audits of pregnancy-related deaths in large hospital systems have identified few abortion-related deaths (Cates et al., 1982).
Some have raised questions regarding CDC’s ability to comprehensively identify abortion-related mortality (Calhoun, 2013; Ferrer, 2020; Hilgers & Horan, 1981; Reardon et al., 2004; Skop, 2023). However, since CDC‘s surveillance of abortion-related mortality began in 1969, critics of CDC’s abortion surveillance have not identified any uncounted abortion-related death, even when offered a financial incentive (Cates et al., 1982).— In 1973, a researcher from the Population Council even went on national television to offer a $100 bounty to anyone who could identify an abortion-related death that had not been counted by the CDC; the bounty went unclaimed even after it was raised to $150 in 1978 (Cates et al., 1982).
Combining data from CDC’s abortion surveillance and NVSS was estimated to ascertain 94% of abortion-related deaths even before the modern PMSS system was implemented (Coble et al., 1992).
PMSS is Better at Capturing All Pregnancy-Related Deaths Than NVSS.PMSS identifies pregnancy related deaths using death records, birth and fetal death records within 1 year of the death, medical records, autopsy reports, media searches, and reporting from public health agencies, health care providers and the public in the identification process, while NVSS uses only the cause of death identified on death certificates (Trost et al., 2022). While NVSS only counts deaths that occur up to six weeks postpartum, PMSS reviews all deaths within 1 year after the end of pregnancy; this timeline allows for a more comprehensive evaluation of all deaths which might be related to pregnancy. Deaths are identified in PMSS by CDC epidemiologists who perform an in-depth review of vital records (e.g., medical records, autopsy reports) for each death. All pregnancy-associated deaths are reviewed to see whether they are pregnancy-related; because PMSS provides a uniform system for identifying pregnancy-related deaths, for all outcomes.
Before 2003 (which overlaps with the analytic period studied in the Raymond and Grimes study), it was well known that pregnancy-related deaths (not related to abortion) were significantly under-reported (Cates et al., 1982; Coble et al., 1992). Compared to PMSS, NVSS (which identifies deaths from cause of death listed on death certificates) is known to significantly undercount pregnancy-related deaths; one study that compared the two systems found that NVSS missed 40% of pregnancy related deaths captured by PMSS (MacKay et al., 2005).
🅑 Summary of Pregnancy Related Mortality Tracking
All pregnancy-related deaths for all pregnancy outcomes, including deaths related to live birth and deaths related to induced abortion are both identified by the Pregnancy Mortality Surveillance System (PMSS).
PMSS uses active epidemiological surveillance, reviewing records of all deaths occurring within a year of pregnancy.
Identification of abortion-related deaths in PMSS is further supplemented by review of associated patient records, birth and fetal death records, medical records, autopsy reports, public health agencies, health care providers and the public media reports, and deaths identified by maternal mortality review committees.
CDC’s tracking of abortion-related deaths does not rely on voluntary reporting from the states.
While no epidemiological surveillance system is perfect, there is no credible evidence to suggest significant underreporting of abortion-related deaths.
⓷ Calculating Relative Risk of Abortion and Live Birth
To calculate the relative risk of live birth and abortion, Raymond and Grimes calculated the mortality rate associated with live birth and the mortality rate associated with legal abortion based on deaths recorded in PMSS. (PMSS data was used for reasons explained above.)
🅐 How Raymond and Grimes Calculated Risk of Death Related to Live Birth
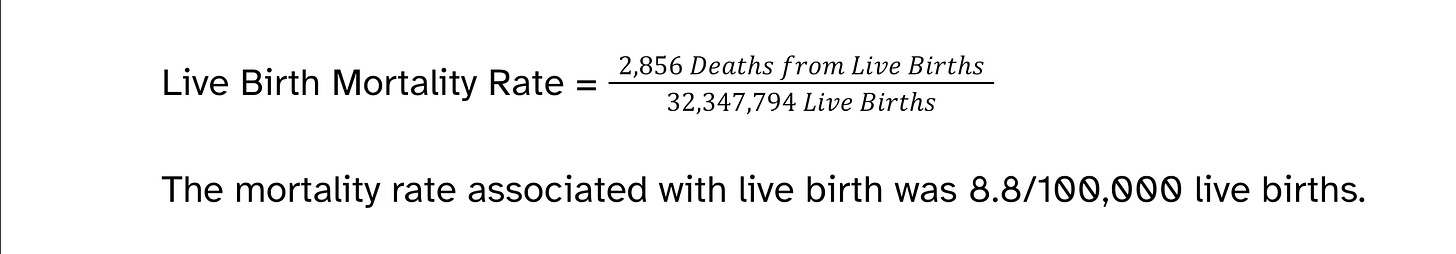
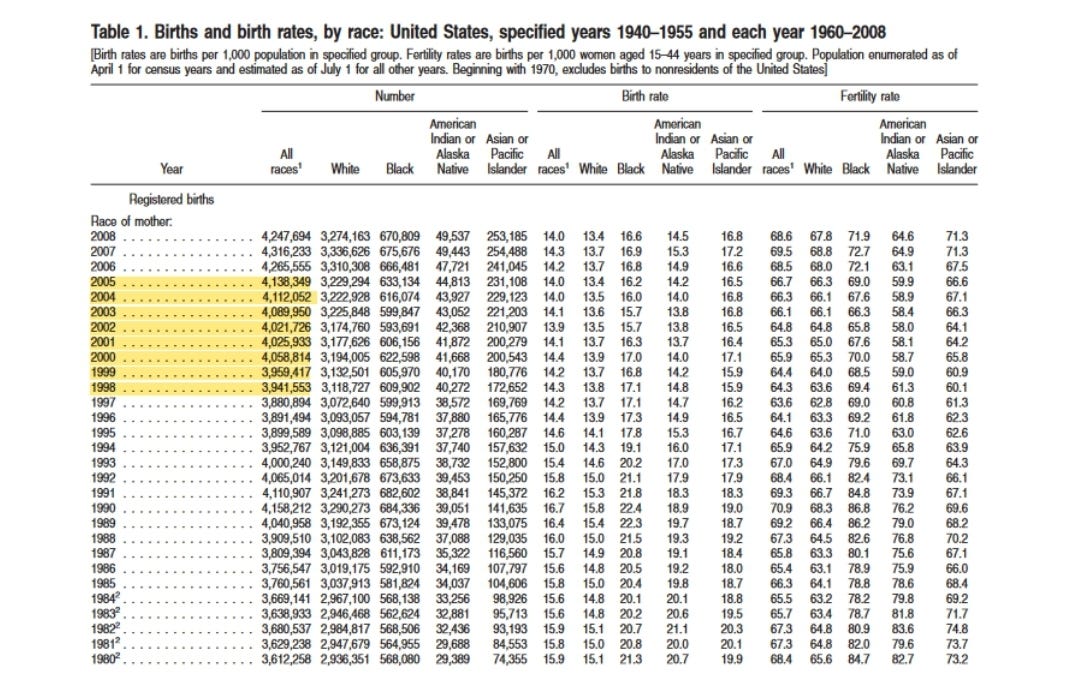
Raymond and Grimes calculated the mortality rate associated with live birth by dividing the number of deaths related to live births (identified in PMSS) from 1998 to 2005 by the number of live births (identified in NVSS) over the same period. 6
From 1998 to 2005, there were 2,856 maternal deaths associated with live birth (Berg et al., 2010) and 32,347,794 live births (Martin et al., 2010). The mortality rate associated with live birth was 8.8 deaths p/ 100,000 live births (Raymond & Grimes, 2012).
🅑 How Raymond and Grimes Calculated the Mortality Rate Related to Legal Abortion
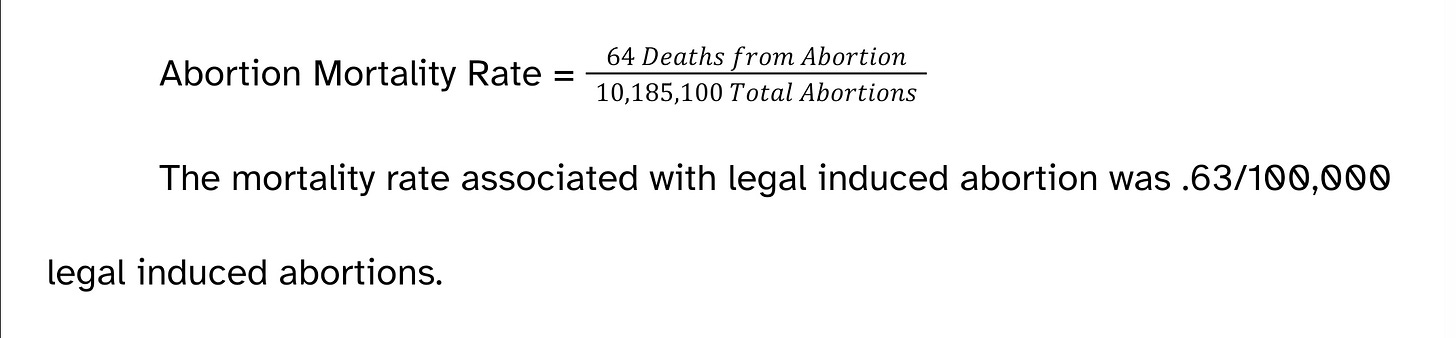
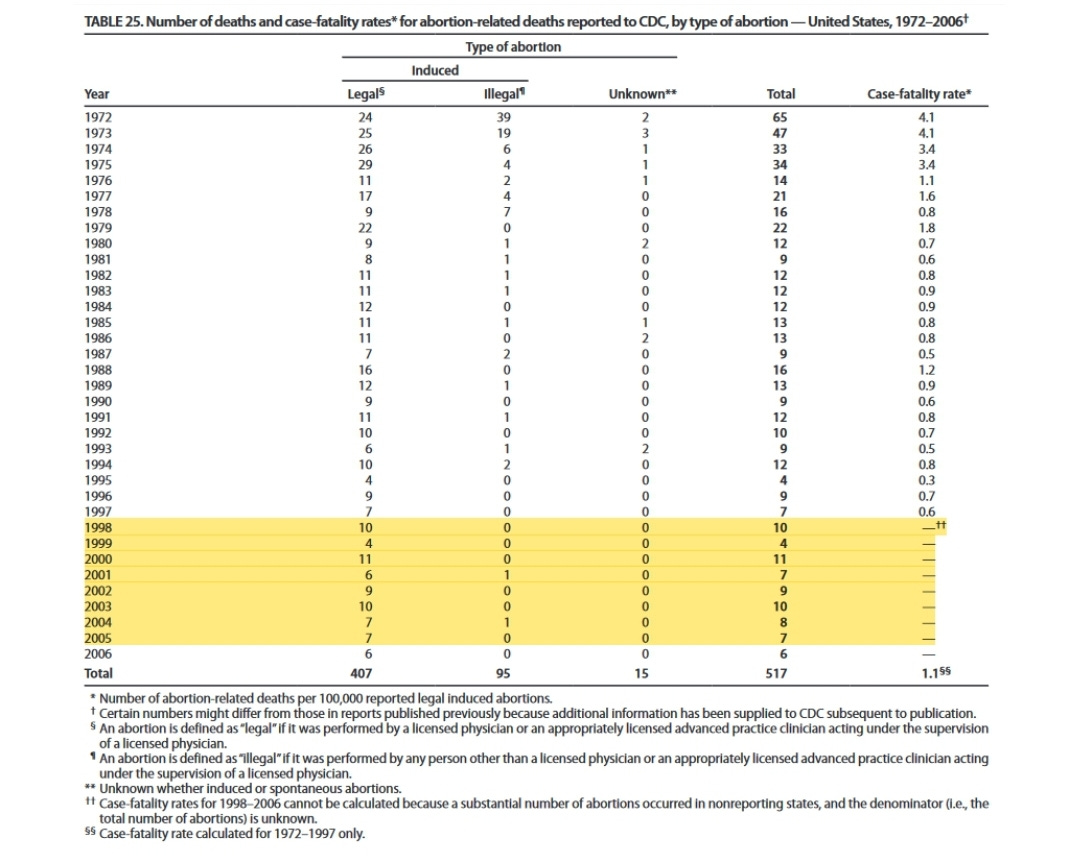
The mortality rate of legal abortion was calculated by the dividing the number of deaths related to legal induced abortion identified in PMSS from 1998 to 2005 by the total number of abortions estimated by the Guttmacher Institute.
Guttmacher Institute’s estimate of the total number of abortions performed was used to calculate legal induced abortion mortality rate because the number of abortions reported to the CDC is known to undercount the number of abortions reported and Guttmacher’s estimate of the total number of abortions performed is more accurate than the number Reported to the CDC.
States report the total number of abortions performed on a voluntary basis. The number of abortions performed by the CDC for the period from 1998 to 2005 is known to undercount of the number of abortions performed because 7 of 52 reporting areas failed to consistently report the number of abortions performed for some or all of the period from 1998 to 2005 to the CDC
Because data from the states is reported voluntarily, and reporting regions may fail to consistently report the number of abortions performed in a given year, CDC has long relied on data collected by Guttmacher Institute,7 a non-profit organization, that surveys every known abortion provider periodically to estimate the number of abortions performed (Jones et al., 2008). Guttmacher Institute’s count is generally considered to be more reliable than the passively reported numbers that states submit to the CDC because Guttmacher collects reports by nationwide survey of all known abortion providers and uses numerous active follow-up methods to increase completeness of the data (Cates et al., 1982; Pazol et al., 2011). The number of abortions reported to Guttmacher Institute are often substantially higher than the number recorded by the CDC; from 1998-2007, the total annual number of abortions recorded by the CDC was only 65%–69% of the number recorded by the Guttmacher Institute (Cates et al., 1982; Pazol et al., 2011).
From 1998 to 2005, there were 64 deaths associated with legal induced abortion (Pazol et al., 2011), and Guttmacher Institute reported 10,185,100 abortions (Jones & Kooistra, 2011).
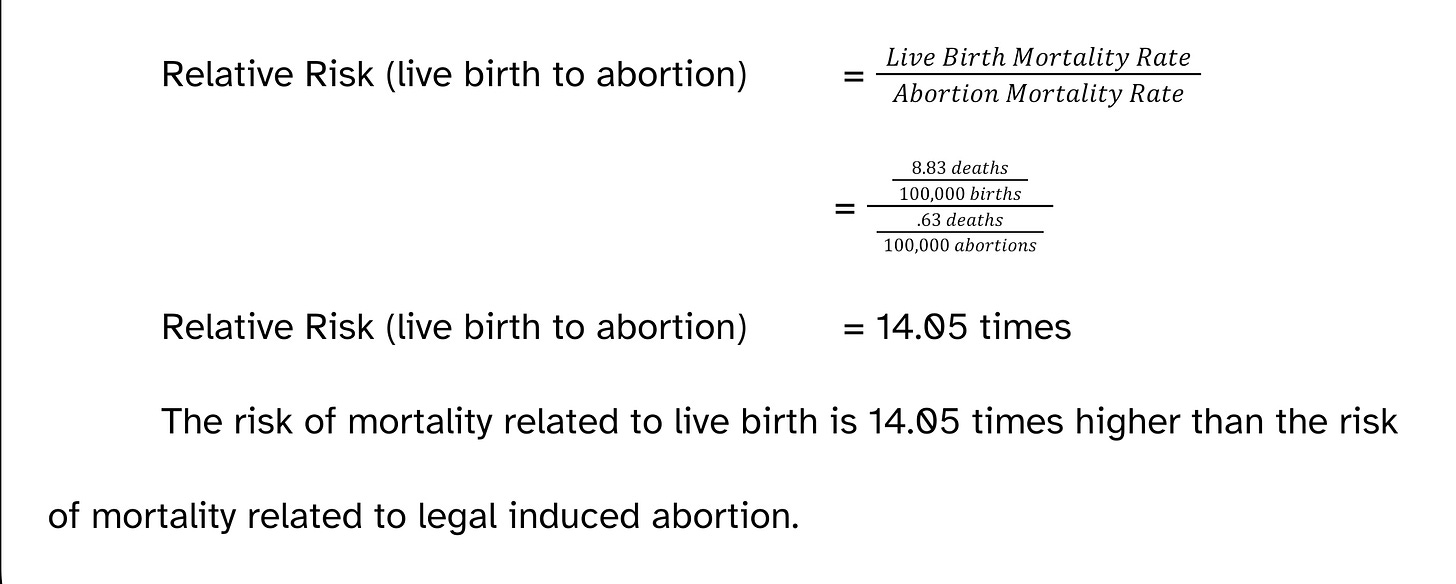
Maternal mortality associated with live birth is 14.05 times higher than mortality associated with legal induced abortion.
🅒 How Raymond and Grimes Calculated the Relative Risk of Live Birth to Legal Induced Abortion
To calculate the relative risk of live birth to abortion, Raymond and Grimes divided the risk of mortality related to live birth by the risk of mortality related to legal induced abortion.
This analysis has both strengths and weaknesses. While PMSS is far more accurate than other systems for tracking maternal related deaths, no epidemiological surveillance system, including PMSS, is perfect. Hence, there may be still be some deaths related to pregnancy that were uncounted. A particular limitation is that the total number of abortions (the denominator of the abortion mortality rate) is estimated. However, it is possible to demonstrate that uncertainty in the data does not change the underlying conclusion: legal induced abortion is safer than live birth.
⓸ Abortion Really is Safer Than Birth
Critics have questioned the analysis by Raymond & Grimes, suggesting that the number of abortion-related deaths are underreported or misreported or the total number of abortions overreported; either might artificially reduce the abortion-mortality rate and impact the relative risk (Calhoun, 2013; Ferrer, 2020; Reardon, 2012; Skop, 2024).
While there is no reason to believe abortion-related deaths are significantly undercounted (Cates et al., 1982; Coble et al., 1992), it is useful to consider how sensitive the relative safety of legal abortion to live birth is to the possibility that abortion-related deaths were undercounted or that the total number of abortions performed was overestimated.
🅐 Legal Induced Abortion is Safer Than Birth Even if the Total Number of Abortions Reported Was Significantly Overestimated
The total number of abortions reported to the CDC cannot be used to generate a valid abortion mortality rate because states do not consistently report abortions to the CDC and are inconsistent in their requirements for abortion reporting (Pazol et al., 2011). In order to calculate the abortion-related mortality rate, CDC uses the number of abortions reported by Guttmacher Institute, based on the institute's survey of abortion providers.
Some critics have suggested (without evidence) that Guttmacher Institute numbers may be an overestimate: if fewer abortions were performed than estimated, the abortion-related mortality rate might seem lower than it is (Calhoun, 2013; Ferrer, 2020; Skop, 2024).
But only 45 of 52 reporting areas were consistently reported by states to the CDC from 1999 to 2005; as such the total number of abortions reported by the states to the CDC is lower than the actual number of abortions performed.— Still, even using this known undercount, the mortality rate associated with legal abortion would be .93 deaths /100,000 legal induced abortions and thus legal induced abortion would still be 9.4 times safer than birth.
🅑 Legal Abortion is Safer Than Pregnancy Even if All Deaths Related to Miscarriage and Illegal Abortion Are Attributed to Legal Induced Abortion
Some critics have expressed concern that deaths related to legal abortion will be misattributed to spontaneous abortion (Ferrer, 2020). Between 1998 and 2005, there were 132 deaths related to spontaneous and induced abortion (Berg et al., 2010).
If all deaths related to illegal abortion and miscarriage are attributed to legal abortion, the abortion mortality rate would be 1.3 deaths /100,000 abortions and legal induced abortion would still be 6.8 times safer than birth.
🅒 Legal Abortion is Safer Than Birth Even if CDC Only Correctly Identified One in Five Deaths Related to Legal Abortion
Some have suggested (without evidence) that abortion-related deaths may be undercounted or misidentified on death certificates because of the stigma associated with abortion (Calhoun, 2013; Ferrer, 2020; Hilgers & Horan, 1981; Reardon, 2012; Skop, 2024). While there is no evidence of substantial underreporting of abortion-related mortality, even if abortion-related mortality were grossly underreported, abortion would still be far safer than live birth.
From 1998 to 2005, CDC identified 64 pregnancy related deaths as related to legal abortion (Pazol et al., 2011). If CDC had only correctly identified one in five abortion-related deaths, there would have been 320 deaths related to legal abortion from 1998 to 2005; CDC would have had to miss 256 deaths related to legal abortion.
Even under the highly unlikely case that CDC only identified one in every five deaths related to legal abortion, live birth would still have carried 2.8 times the risk of death related to legal abortion.
🅓 Induced Abortion is Safer Than Pregnancy Even if the Total Number of Abortions Reported Were Too High and Abortion-Related Deaths Are Underreported
Even in the extremely implausible circumstance that only one in five abortion-related mortalities were correctly identified by the CDC and even undercounting the number of abortions performed, the induced abortion mortality rate would still be 1.88 times less than the live birth mortality rate.
🅔 For Live Birth to Even Be Equally as Safe as Legal Abortion, CDC Would Have to Significantly Undercount Deaths Related to Legal Abortion.
For live birth to even be equally as safe as legal abortion (have the same risk of death), the CDC would have had to failed to identify 835 deaths that were caused by or arising from conditions related to abortion as “abortion-related.” For this to be plausible, the CDC would have had to correctly identified and counted only one in every fourteen abortion-related deaths. Selective underreporting of deaths related to legal abortion cannot account for a difference this large.
⓹ Summary
Abortion would still be safer than pregnancy:
Even if far fewer abortions were performed than estimated
Even if all deaths identified as related to miscarriage or illegal abortion were really caused by legal abortion
Even if CDC only correctly identified one in every five abortion-related deaths (five times as many people died from legal abortion)
Even if CDC only correctly identified one in every five legal abortion-related deaths and far fewer legal abortions were performed than estimated
Even though it is not possible to be certain that CDC did not fail to identify some deaths related to abortion, even though it is not possible to know exactly how many abortions were performed in the US from 1998 to 2005,8 by analyzing how the relative risk live birth to abortion would be affected by the underreporting of abortion-related deaths or overestimating the number of abortions, or both, it can be demonstrated that under every remotely plausible scenario, legal induced abortion has a far lower mortality rate than live birth.■
Sources, sourced data, and footnotes can be found below.
⓺ Sources, Sourced Data, and Footnotes
In-text Sources
Berg, C. J., Callaghan, W. M., Syverson, C., & Henderson, Z. (2010). Pregnancy-Related Mortality in the United States, 1998 to 2005. Obstetrics & Gynecology, 116(6), 1302–1309. https://doi.org/10.1097/AOG.0b013e3181fdfb11
Calhoun, B. (2013). The Maternal Mortality Myth in the Context of Legalized Abortion. The Linacre Quarterly, 80(3), 264–276. https://doi.org/10.1179/2050854913Y.0000000004
Cates, W., Jr, Smith, J. C., Rochat, R. W., & Grimes, D. A. (1982). Mortality From Abortion and Childbirth: Are the Statistics Biased? JAMA, 248(2), 192–196. https://doi.org/10.1001/jama.1982.03330020036026
Centers for Disease Control & Prevention. (2024, May 20). Pregnancy Mortality Surveillance System. Maternal Mortality Prevention. https://www.cdc.gov/maternal-mortality/php/pregnancy-mortality-surveillance/index.html
Coble, Y. D., Jr, Estes, E. H., Jr, Head, C. A., Karlan, M. S., Kennedy, W. R., Numann, P. J., Scott, W. C., Skelton, W. D., Steinhilber, R. M., Strong, J. P., Toevs, C. C., Wagner, H. N., Jr, Loeb, J. M., Rinaldi, R. C., & Gans, J. E. (1992). Induced Termination of Pregnancy Before and After Roe v Wade: Trends in the Mortality and Morbidity of Women. JAMA, 268(22), 3231–3239. https://doi.org/10.1001/jama.1992.03490220075032
Ferrer, D. J. (2020, February 27). Is Abortion 14 Times Safer Than Childbirth? Equal Rights Institute Blog. https://blog.equalrightsinstitute.com/is-abortion-14-times-safer-than-childbirth/
Gerberding, J. (2004, July 20). CDC Response to Walter Weber Regarding Maternal Mortality Statistics. http://afterabortion.org/pdf/CDCResponsetoWeberReAbortionStats-Gerberding%20Reply.pdf
Grimes, D. A. (2006). Estimation of pregnancy-related mortality risk by pregnancy outcome, United States, 1991 to 1999. American Journal of Obstetrics and Gynecology, 194(1), 92–94. https://doi.org/10.1016/j.ajog.2005.06.070
Guttmacher Institute. (2015, November 20). About. https://www.guttmacher.org/about
Hilgers, T. W., & Horan, D. J. (1981). Abortion-related maternal mortality: An in-depth analysis. In T. W. Hilgers, D. J. Horan, & D. Mall (Eds.), New perspectives on human abortion (pp. 69–91). University Publications of America.
Jones, R. K., & Kooistra, K. (2011). Abortion Incidence and Access to Services In the United States, 2008. Perspectives on Sexual and Reproductive Health, 43(1), 41–50.
Jones, R. K., Zolna, M. R. S., Henshaw, S. K., & Finer, L. B. (2008). Abortion in the United States: Incidence and Access to Services, 2005. Perspectives on Sexual and Reproductive Health, 40(1), 6–16.
MacKay, A. P., Berg, C. J., Duran, C., Chang, J., & Rosenberg, H. (2005). An assessment of pregnancy-related mortality in the United States. Paediatric and Perinatal Epidemiology, 19(3), 206–214. https://doi.org/10.1111/j.1365-3016.2005.00653.x
Martin, J. A., Hamilton, B. E., Sutton, P. D., Ventura, S. J., Mathews, T. J., & Osterman, M. J. K. (2010). Births: Final data for 2008. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 59(1), 1, 3–71.
National Center for Health Statistics. (2024, May 9). NVSS - Maternal Mortality—FAQ. https://www.cdc.gov/nchs/maternal-mortality/faq.htm
Pazol, K., Creanga, A. A., & Zane, S. B. (2012). Trends in use of medical abortion in the United States: Reanalysis of surveillance data from the Centers for Disease Control and Prevention, 2001–2008. Contraception, 86(6), 746–751. https://doi.org/10.1016/j.contraception.2012.05.023
Pazol, K., Zane, S., Parker, W. Y., Hall, L. R., Gamble, S. B., Hamdan, S., Berg, C., Cook, D. A., & Centers for Disease Control and Prevention (CDC). (2011). Abortion surveillance—United States, 2007. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 60(1), 1–42.
Raymond, E. G., & Grimes, D. A. (2012). The Comparative Safety of Legal Induced Abortion and Childbirth in the United States. Obstetrics & Gynecology, 119(2 Part 1), 215–219. https://doi.org/10.1097/AOG.0b013e31823fe923
Reardon, D. C. (2012). Rebuttal of Raymond and Grimes. The Linacre Quarterly, 79(3), 259–260. https://doi.org/10.1179/002436312804872730
Reardon, D. C., Strahan, T. W., Thorp, J. M., & Shuping, M. W. (2004). Deaths associated with abortion compared to childbirth—A review of new and old data and the medical and legal implications. The Journal of Contemporary Health Law and Policy, 20(2), 279–327.
Rochat, R. W., Heath, C. W., Jr, Chu, S. Y., & Marchbanks, P. A. (2011). Maternal and Child Health Epidemic-Assistance Investigations, 1946–2005. American Journal of Epidemiology, 174(suppl_11), S80–S88. https://doi.org/10.1093/aje/kwr304
Skop, I. (2023, January 6). Handbook of Maternal Mortality: Addressing the U.S. Maternal Mortality Crisis, Looking Beyond Ideology. Lozier Institute. https://lozierinstitute.org/handbook-of-maternal-mortality-addressing-the-u-s-maternal-mortality-crisis-looking-beyond-ideology/
Skop, I. (2024, April 25). Fact Check: “Abortion is 14 Times Safer than Childbirth.” Lozier Institute. https://lozierinstitute.org/fact-check-abortion-is-14-times-safer-than-childbirth/
Trost, S. L., Beauregard, J., Petersen, E. E., Cox, S., Chandra, G., St. Pierre, A., Rodriguez, M., & Goodman, D. (2022). Identifying Deaths During and After Pregnancy: New Approaches to a Perennial Challenge. Public Health Reports, 138(4), 567–572. https://doi.org/10.1177/00333549221110487
WHO, UNICEF, UNFPA, World Bank Group, & UNDESA/Population Division. (2023). Trends in maternal mortality 2000 to 2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. https://www.who.int/publications-detail-redirect/9789240068759
Sources for the Raymond and Grimes Numbers
Pregnancy-related Deaths by Outcome of Pregnancy, 1998-2005
(Please note "Abortion" refers to both spontaneous and induced abortion)
Berg, C. J., Callaghan, W. M., Syverson, C., & Henderson, Z. (2010). Pregnancy-related mortality in the United States, 1998 to 2005. Obstetrics and gynecology, 116(6), 1302–1309. https://doi.org/10.1097/aog.0b013e3181fdfb11
2,856 pregnancy-related deaths ending in live births (1998-2005)
132 pregnancy-related deaths ending in induced or spontaneous abortion (1998-2005)
Births and birth rates, by race, United States, specified years, 1940-1955 and each 1980-2008
Martin, J. A., Hamilton, B. E., Sutton, P. D., Ventura, S. J., Mathews, T. J., & Osterman, M. J. (2010). Births: final data for 2008. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 59(1), 1–71.
32,347,794 live births (1998 - 2005)
Number of deaths and case-fatality rates for deaths reported to CDC, by type of abortion, United States, 1972-2006
Pazol, K., Zane, S., Parker, W. Y., Hall, L. R., Gamble, S. B., Hamdan, S., Berg, C., Cook, D. A., & Centers for Disease Control and Prevention (CDC) (2011). Abortion surveillance - United States, 2007. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002), 60(1), 1–42.
64 deaths associated with legal abortion
2 deaths related to illegal abortion
66 deaths related to spontaneous abortion
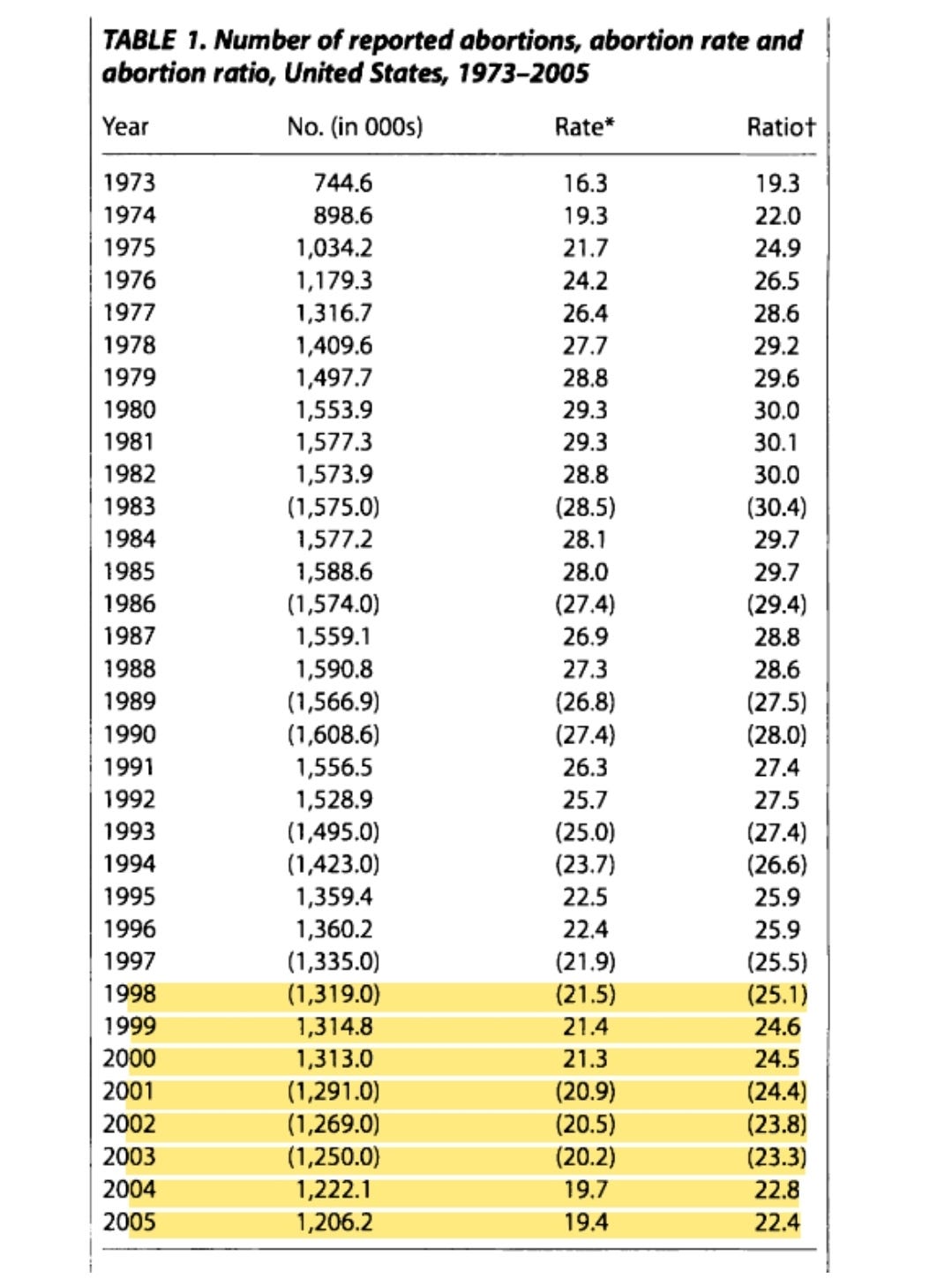
Number of reported abortions, abortion rate and abortion ratio, United States, 1973-2005
Jones, R. K., Zolna, M. R. S., Henshaw, S. K., & Finer, L. B. (2008). Abortion in the United States: Incidence and Access to Services, 2005. Perspectives on Sexual and Reproductive Health, 40(1), 6–16. https://doi.org/10.1363/4000608
10,185,100 Total Abortions based on Guttmacher Institute (1998-2005)
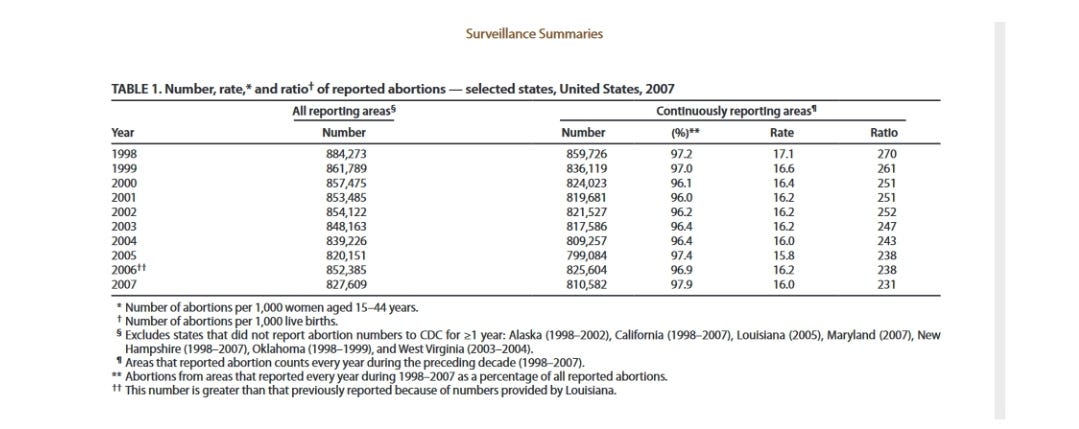
Number, rate and ratio of reported abortions - selected states, United States, 2007
Pazol, K., Zane, S., Parker, W. Y., Hall, L. R., Gamble, S. B., Hamdan, S., Berg, C., Cook, D. A., & Centers for Disease Control and Prevention (CDC) (2011). Abortion surveillance - United States, 2007. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C. : 2002), 60(1), 1–42.
6,818,024 total abortions reported to CDC (1998-2005)
Footnotes
MMRIA is used to conduct surveillance at the state and local levels through state maternal mortality committees (Trost et al., 2022). MMRCs provide more in-depth review of non-medical records and conduct interviews them to review injury deaths, namely suicides and overdoses, which are excluded from the deaths reported by NVSS and PMSS. However, MMRCs are the most time and resource-intensive tracking methods and do not have uniform processes or funding, which can lead to substantial differences in timeliness, and identification methods across jurisdictions.
Deaths within a year of pregnancy but not caused by pregnancy are “pregnancy associated deaths” but not “pregnancy-related deaths.”
130 deaths were not pregnancy-associated (occurring more than 1 year after the end of pregnancy). In 14 cases, either the temporal or causal relationship between the death and pregnancy could not be determined (Berg et al., 2010).
For 1998 to 2005, a majority of unknown deaths were suggestive of a death in the latter half of pregnancy but CDC researchers were unable to find a matching birth certificate or fetal death certificate so it is unclear whether these deaths were stillbirths or live births (Berg et al., 2010).
While abortion-related deaths have been identified using the Pregnancy Mortality Surveillance System since 1987, CDC has used active epidemiological surveillance methods to monitor deaths related to abortion since 1969 (Pazol et al., 2011, 2012).
These deaths exclude deaths related to stillbirths, ectopic pregnancies, undelivered pregnancies, trophoblastic pregnancies and pregnancies with unknown outcomes(Berg et al., 2010).
he Guttmacher Institute is “a leading research and policy organization committed to advancing sexual and reproductive health and rights (SRHR) worldwide” (Guttmacher Institute, 2015). Guttmacher Institute supports abortion rights.
The total number of abortions reported by the CDC must be an undercount, because only 45 of 52 reporting areas consistently reported abortions to the CDC during the period analyzed by Raymond and Grimes (Pazol et al., 2011).



It is odd that this author is aware of several of my older reviews of the literature but chose not to discuss my 2017 review which demonstrates that analyses from countries with record linkage data clearly demonstrate higher rates of mortality associated with abortion...especially from suicide, accidents, risk taking behavior and longer term cardiovascular diseases. See https://pubmed.ncbi.nlm.nih.gov/29163945/